Imagine opening your annual health insurance renewal notice expecting a modest increase, only to find your premium has effectively doubled. That's the sticker shock facing millions of Americans as the 2026 Affordable Care Act open enrollment period unfolds, with coverage costs nationwide experiencing their sharpest spike in nearly a decade.
The open enrollment period that began November 1, 2025, has revealed a drastic surge in coverage costs driven by two converging factors: the largest insurance rate increases since 2018 and Congress's failure to extend critical premium tax credits in the partisan 2025 budget bill. The result is an affordability crisis that experts warn will leave at least 4.2 million Americans without health insurance coverage.
"We're seeing the perfect storm of policy failure and market dynamics colliding at the worst possible time for consumers," said healthcare policy analysts tracking the enrollment period. The Congressional Budget Office projects the coverage losses as a direct consequence of the enhanced premium tax credit expiration included in House Resolution 1, the budget reconciliation bill passed along party lines earlier this year.
Historic Rate Increases Compound Subsidy Loss
Insurance companies across the country submitted rate filings for 2026 that mark the most significant premium increases the ACA marketplaces have experienced since 2018, when the individual mandate penalty was eliminated. State insurance departments approved median rate increases of 18 percent, though some states saw proposals exceeding 25 percent for benchmark silver plans.
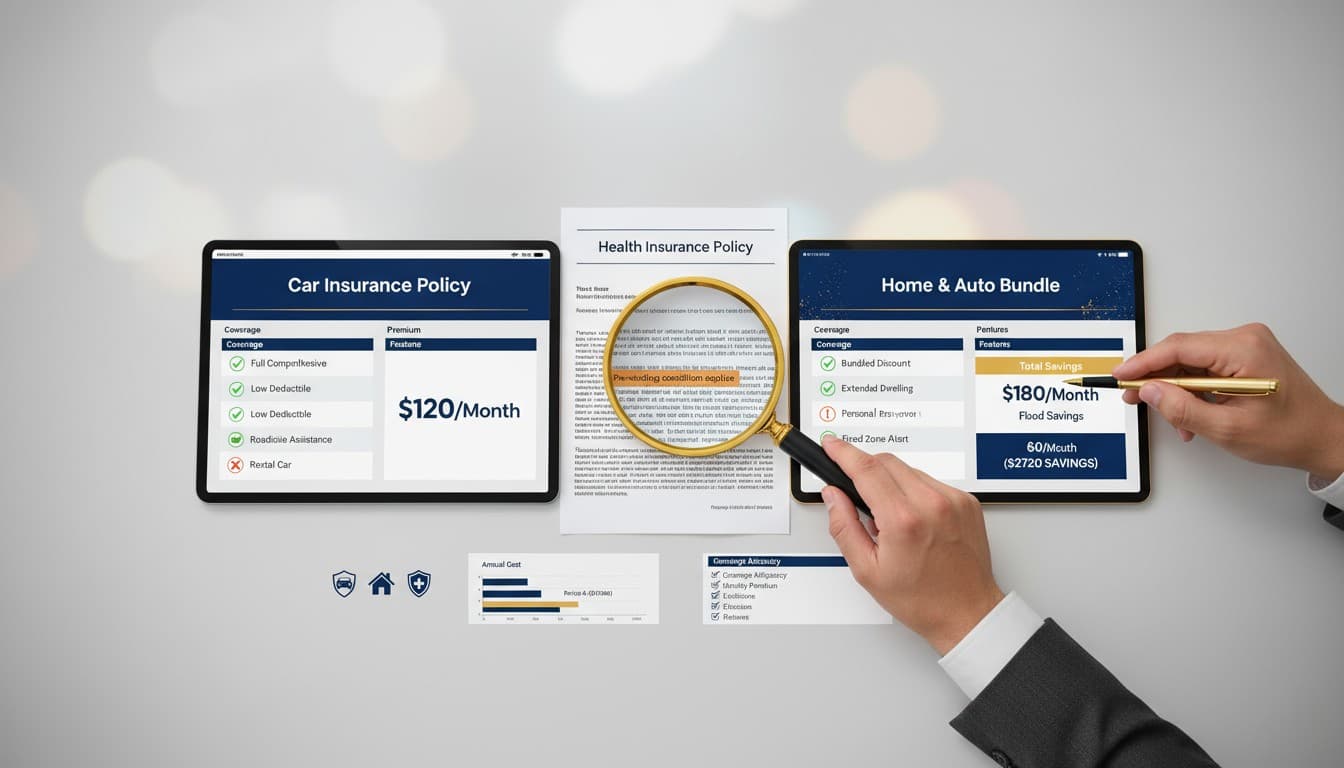
The rate increases alone would have created affordability challenges for many enrollees. However, the simultaneous expiration of enhanced premium tax credits—which had made coverage significantly more affordable since 2021—compounds the impact exponentially for subsidized consumers.
For enrollees who receive federal premium assistance, the subsidy amount is calculated based on the difference between the benchmark plan cost and a percentage of their household income. When both the benchmark cost rises and the subsidy formula reverts to pre-2021 levels, consumers face increases from both directions.
Industry representatives cite several factors driving the rate increases. Rising medical costs, including increased utilization of healthcare services as pandemic-era delays in care reverse, have pushed claims higher. Inflation affecting labor costs for healthcare providers has been passed through to insurance premiums. Additionally, pharmacy costs, particularly for specialty medications and new treatments, continue to escalate.
Open Enrollment Data Reveals Consumer Impact
The Centers for Medicare & Medicaid Services, which administers HealthCare.gov for states using the federal marketplace platform, reported unprecedented call volume during the first week of open enrollment. Consumer assistance centers and insurance navigators described fielding thousands of calls from confused and distressed enrollees seeking to understand why their costs had increased so dramatically.
State-based marketplaces reported similar experiences. California's Covered California marketplace noted that many consumers were unaware the enhanced subsidies they had received for the past several years were temporary and required Congressional renewal. New York's marketplace reported that enrollment assisters were spending significantly more time with each consumer as people explored lower-cost plan options or considered dropping coverage entirely.
Insurance brokers who work with marketplace consumers described difficult conversations with clients who had successfully maintained coverage for years but now questioned whether they could afford to continue. Many consumers are considering switching from preferred provider organization plans to health maintenance organization plans with more limited networks, or selecting plans with higher deductibles to reduce monthly premium costs.
"The most heartbreaking conversations are with people who did everything right—they enrolled in coverage, paid their premiums, used preventive care—and now they're being priced out through no fault of their own," said one enrollment counselor based in Florida.
Geographic and Demographic Disparities
The impact of the rate increases and subsidy expiration varies significantly based on geography, income level, age, and family composition. Analysis of marketplace data reveals stark disparities in how different populations are affected.
Rural areas, which already faced higher baseline premiums due to limited insurer competition and costlier healthcare delivery, are experiencing particularly severe impacts. Some rural counties have only one insurer offering marketplace plans, eliminating consumers' ability to shop for better rates.
Older adults who have not yet reached Medicare eligibility at age 65 face the steepest premium increases in dollar terms. Age-based rating rules allow insurers to charge older adults up to three times what they charge younger adults, meaning a 64-year-old's premium increase will be substantially larger than a 30-year-old's, even if the percentage increase is identical.
Middle-income families—particularly those earning between 400 and 600 percent of the federal poverty level—face especially dramatic changes. Under the enhanced premium tax credits, these families qualified for subsidies that made coverage affordable. With the credits expired, many now receive no federal assistance at all, leaving them to pay full premium costs that can exceed $1,500 monthly for family coverage in high-cost areas.
Self-employed individuals and small business owners, who lack access to employer-sponsored coverage, represent a significant portion of marketplace enrollees and are disproportionately affected by the affordability crisis. This population includes freelancers, gig economy workers, and entrepreneurs whose income may fluctuate, making it difficult to budget for dramatically higher insurance costs.
Congressional Failure and Political Dynamics
The enhanced premium tax credits became a casualty of the intense partisan dispute over the 2025 budget reconciliation bill. Democrats sought to include an extension of the subsidies, arguing they represented critical support for working families and small business owners. Republicans opposed the inclusion, citing concerns about federal spending levels and the long-term cost of the subsidies.
The final budget bill that passed Congress did not include the enhanced premium tax credit extension. Democratic leaders accused Republicans of abandoning millions of Americans who depend on marketplace coverage. Republican leaders countered that the subsidies were always intended as temporary pandemic relief and that their continuation represented an expansion of government spending the nation could not afford.
Some moderate Republicans, particularly those representing districts with high marketplace enrollment, reportedly supported extending the subsidies but faced pressure from leadership and conservative caucus members to oppose any additions to the budget bill. Several senators indicated they might support standalone legislation to address the subsidy expiration, but no such bill has advanced through committee.
President Trump, in comments during the ongoing government shutdown, suggested a different approach entirely. He proposed redirecting the funding currently used for marketplace subsidies into direct payments to individuals, allowing them to purchase coverage outside the marketplace structure. The proposal has not been developed into specific legislation and has received mixed responses from health policy experts.
Industry Concerns About Market Stability
Insurance companies and industry organizations have expressed concern that the sudden affordability shock could destabilize the individual insurance market. The cycle of adverse selection—where healthier people drop coverage due to cost, leaving a sicker risk pool that drives premiums even higher—poses a significant risk to market sustainability.
America's Health Insurance Plans, the national trade association representing insurers, called on Congress to provide immediate clarity on subsidy policy. The organization warned that continued uncertainty could lead insurers to exit markets or submit even higher rate proposals for 2027, anticipating a riskier enrollment pool.
State insurance regulators have also voiced concerns. The National Association of Insurance Commissioners issued guidance to state insurance departments on monitoring enrollment patterns and insurer participation to identify early warning signs of market deterioration. Several state commissioners have urged their Congressional delegations to take action to stabilize the marketplaces.
Some insurers have already indicated they are reassessing their marketplace participation for 2027. While no major exits have been announced, industry analysts note that insurers' willingness to offer coverage depends on their ability to price policies adequately and maintain a balanced risk pool.
Impact on Healthcare Providers and Safety Net
Healthcare providers and hospitals anticipate increased financial strain as patients lose coverage or reduce their utilization of care to manage costs. Uninsured patients are more likely to delay or forgo necessary care, leading to more serious health problems that ultimately require more expensive treatment.
Federally Qualified Health Centers, which serve as primary care safety net providers for underserved communities, expect increased demand from newly uninsured individuals. However, these centers face capacity constraints and may struggle to accommodate significantly higher patient volumes.
Hospital emergency departments, which cannot turn away patients regardless of insurance status, may see increased uncompensated care costs. The American Hospital Association has warned that coverage losses could undermine the financial stability of hospitals, particularly those serving rural or economically distressed communities.
Public health experts warn that coverage losses will lead to gaps in preventive care, delayed diagnoses of serious conditions, and poorer health outcomes across populations. Chronic disease management, cancer screenings, and mental health treatment are particularly vulnerable to disruption when patients lose coverage or reduce care utilization due to cost concerns.
Special Enrollment Considerations and Deadlines
Consumers currently enrolled in marketplace coverage who take no action will have their coverage automatically renewed, but at the higher premium costs. Those who wish to change plans or explore other options have until January 15, 2026, to enroll in coverage beginning February 1.
Special enrollment periods remain available for individuals who experience qualifying life events such as job loss, marriage, birth of a child, or residential moves. However, simply facing higher costs does not qualify as a special enrollment trigger, meaning most consumers must wait until the annual open enrollment period to make changes.
Some consumers are exploring alternative coverage options. Short-term health plans, which are not required to comply with ACA coverage standards and often exclude pre-existing conditions, have seen increased inquiries. However, consumer advocates warn that these plans provide significantly less comprehensive protection than ACA-compliant coverage.
Healthcare sharing ministries, which are not insurance but rather cost-sharing arrangements typically among members of faith communities, have also reported increased interest. These arrangements are not regulated as insurance and provide no guarantee of payment for medical expenses, making them a risky option for families with significant healthcare needs.
Future Outlook and Potential Solutions
Health policy experts have proposed various approaches to address the affordability crisis. Options range from restoring the enhanced premium tax credits in their original form to creating a permanent subsidy structure that doesn't require periodic Congressional renewal.
Some proposals would extend subsidies only for lower-income enrollees while allowing them to expire for higher-income families. Others would tie subsidy levels to inflation or premium growth, automatically adjusting assistance to maintain affordability without requiring annual Congressional action.
Broader reforms, such as creating a public option plan that would compete with private insurers, or allowing individuals to buy into Medicare before age 65, have been proposed as longer-term solutions. However, such significant policy changes appear unlikely in the current political environment.
What Happens Next
The coming weeks will provide crucial data on how consumers respond to the dramatic cost increases. Early enrollment figures, expected in mid-December, will indicate whether the Congressional Budget Office's projection of 4.2 million coverage losses is accurate or whether the impact will be even more severe.
Healthcare advocates, consumer organizations, and medical provider groups continue to pressure Congress to take action before the enrollment period closes. However, with the government shutdown ongoing and deep partisan divisions over healthcare policy, prospects for quick Congressional action remain uncertain.
For millions of Americans, the situation requires immediate personal decisions: pay significantly more for coverage, switch to less comprehensive plans, or go without insurance and hope for the best. Whatever they choose, the consequences of this policy failure will echo through American healthcare for years to come.